In Sonography, Comfort is Health
Sonographers Have a Higher Risk of Suffering From Work-Related Musculoskeletal Disorders
According to an article published in Reports in Medical Imagingin 2014, work-related musculoskeletal disorders (WRMSDs) are characterized by conditions that are caused or aggravated by performing workplace activities. These conditions, also commonly known as repetitive strain injury, repetitive motion injury, and cumulative trauma disorder, not only affects the sonographer, but also the workplace and patient care (Coffin 15).
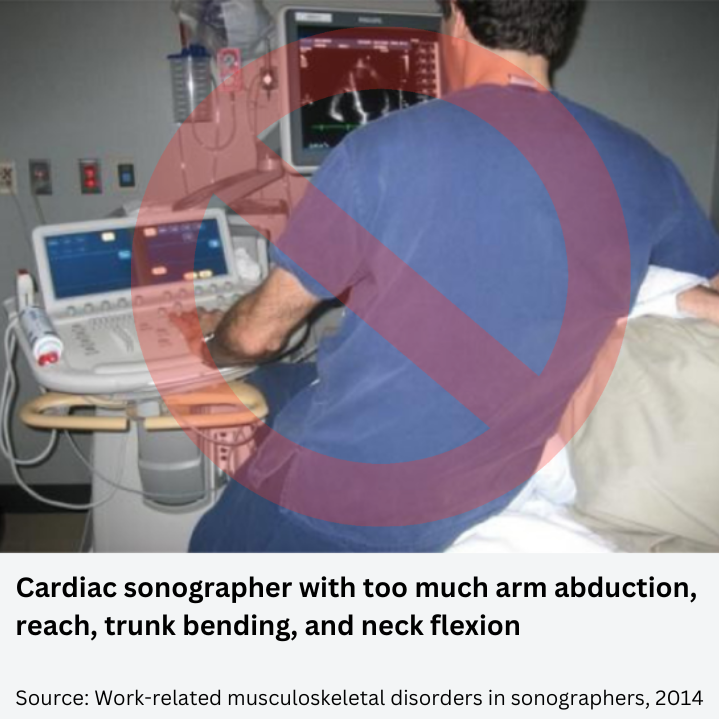
Source: Work-related musculoskeletal disorders in sonographers, 2014
An article published in International Journal of Industrial Ergonomics in 2010, reported that 86% of sonographers reported upper extremity musculoskeletal pain (Burnett and Campbell-Kyureghyanb 306). In the same line, Reports in Medical Imaging explained the most common types of injuries suffered by these medical imaging professionals. The shoulder is a frequent injured body part with conditions that include bursitis, tendonitis and rotator cuff tears (Coffin 17).
Other common injuries that can bee seen among sonographers are tendonitis and tenosynovitis in hands and wrists, as a result of ultrasound transducer gripping. Besides these, nerve entrapment syndromes, such as carpal tunnel syndrome, cubital syndrome, and thoracic outlet syndrome are other common injuries that have a high incidence in ultrasound users. (Coffin 18).
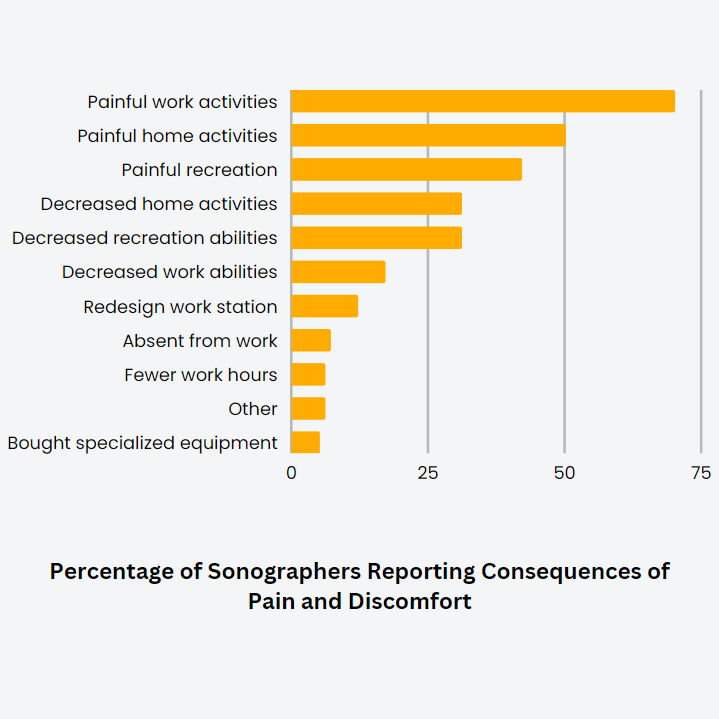
How Do WRMSDs Affect the Personal and Work Life of Sonographers?
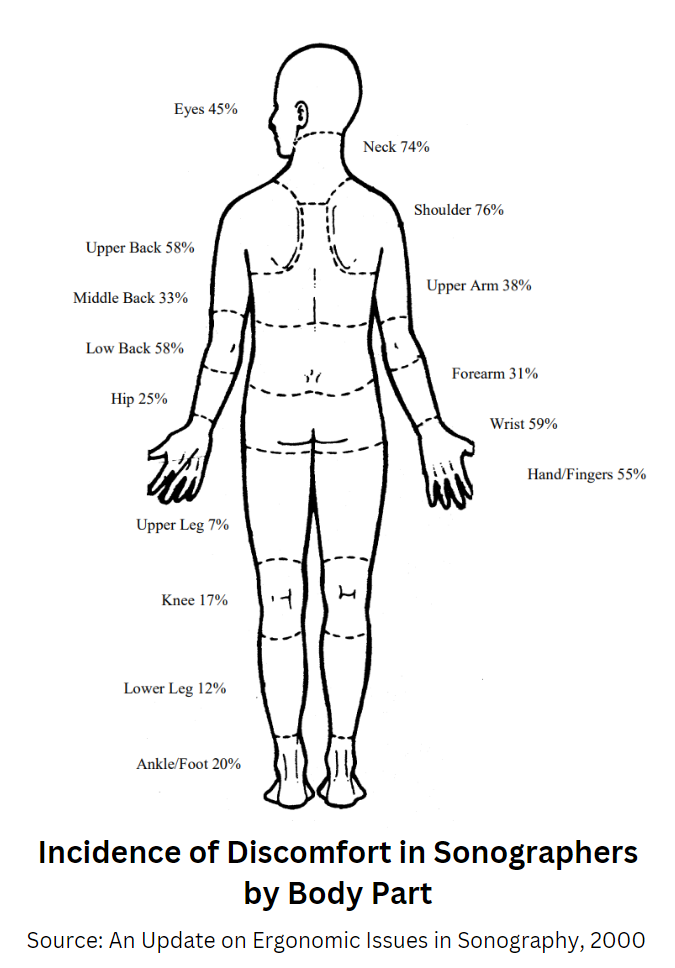
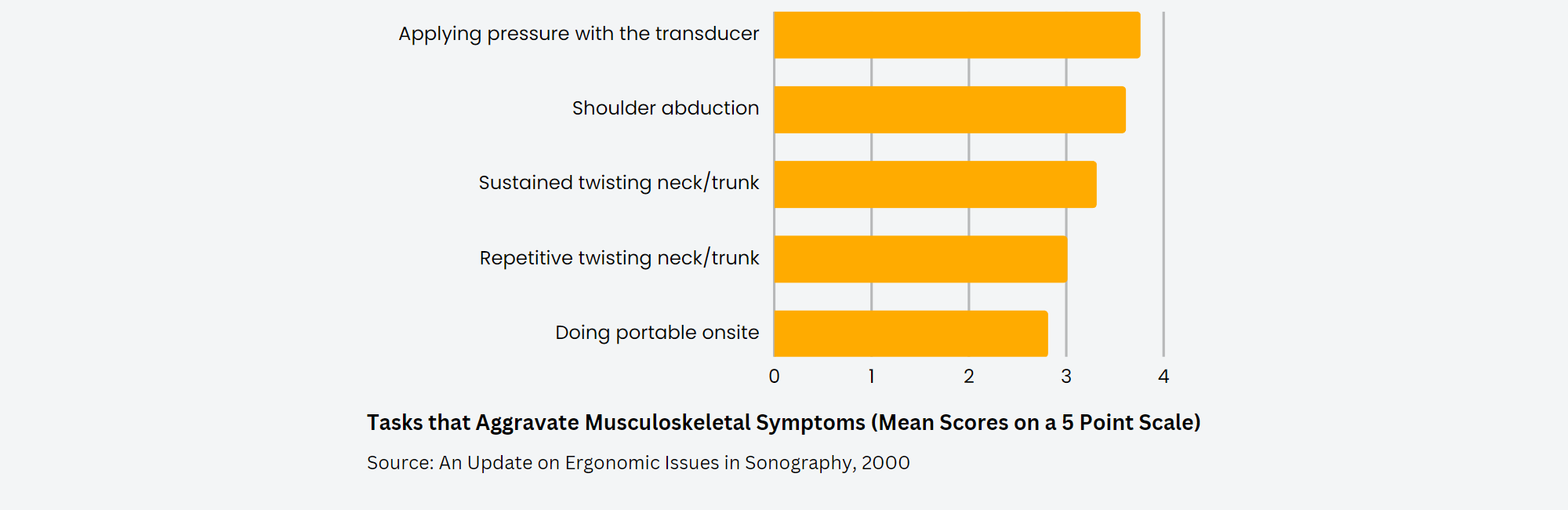
Source: An Update on Ergonomic Issues in Sonography, 2000
WRMSDs Affect the Sonographer's Pockets and the Employer's Budget
In an article published in Journal of Diagnostic Medical Sonography in 2017, the author explained that work-related musculoskeletal disorders are one of the most common reported causes of limited or lost work time, causing employers a burden cost of up to $20 billion every year (Murphey 356).
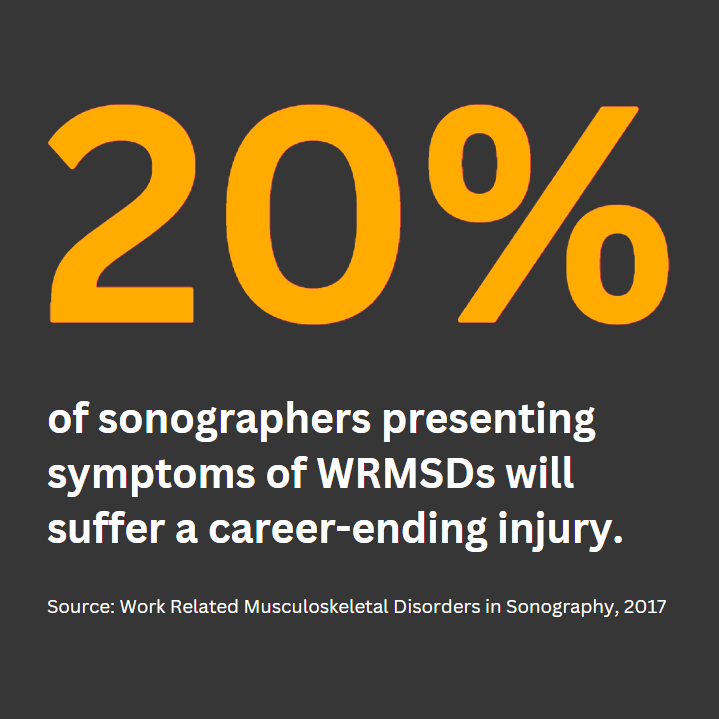
For sonographers, a WRMSD can be a minor discomfort but it can also develop into an injury that could end his or her career.
The beginning of WRMSDs can start as early as 6 month from the employment date in 15% or sonographers. This number increases to 45% after 3 years and reaches up to 72% after 10 years.
According to an article published in Journal of Diagnostic Medical Sonography in 2015, an injured sonographer can represent a cost of over a half million dollars per year. This amount can be distributed in different aspects including:
What Causes WRMSDs in Sonographers
There are several factors that contribute to the development of injuries in ultrasound users. However, most of them can be distributed into these three categories:
- Biomechanical and environmental factors including the workstation, equipment, ultrasound system, and the exam room layout.
- Administrative components such as sonographers tight rotation schedules, high amount of examinations assigned per day and the excessive use of point-of-care ultrasound (POCUS) instead of transporting patients to an ultrasound department.
- Sonographers practices like postures ultrasound professionals use when scanning (Coffin 17). In this category there are other factors that can also affect the health of practitioners, and if they don't perform their duties in a conscious way, the risk of injury can be imminent.
Work Postures Don’ts
The author of the study published in Reports in Medical Imaging explained that one of the most common static posture sonographers adopt is "abduction of either the scanning arm or the non-scanning arm." According to the same article, an abduction angle greater than 30° increases the risk of injury of the shoulder and if the position is maintained for long periods of time, the risk is even higher.
Over-reaching due to the abscence of time to optimize the equipment and adapt it to the examination and patient, is another frequent posture that also induces injuries (Coffin 18).

There are some ultrasound examinations, such as venous reflux, that are usually performed by sonographers with the patient standing on the floor or on a stool, forcing the practitioner to sit or kneel on the floor to have access to the scanning area. This posture results in excessive reach, neck tension and trunk twist (Coffin 18).
Besides excessive abduction and over-reaching, doing ultrasound screenings with the scanning arm behind the shoulder and without support adds strain on the shoulder joint. Also, transducers that require a "pinch' grip instead of a whole-hand or palmar grip, force sonographers to use smallest muscles and demand up to five times more muscle and tendon strength (Coffin 19).
As a sonographer, Jenny understands the challenges you have to face every day and thanks to her experience over the years, she has mastered and overcame the most common ergonomic issues in the ultrasound field. Keep scrolling to find her best recommendations.
Work Postures Dos
- Sonograhers should sit and stand in a way that allows them to move down the length of the exam table to prevent them from reaching back while scanning.
- They should be in front of the most used keys on the ultrasound control panel to avoid reaching across their bodies.
- Strain on the shoulder can be decreased by using an arm support device while using the transducer.
The author in the study published in Reports in Medical Imaging in 2014, explained that arm abduction and over-reaching can be reduced with simple adjustments such as lowering the exam table or raising the chair, and moving the patient and the ultrasound system’s control panel closer to the sonographer (Coffin 19).

Source: Work-related musculoskeletal disorders in sonographers, 2014
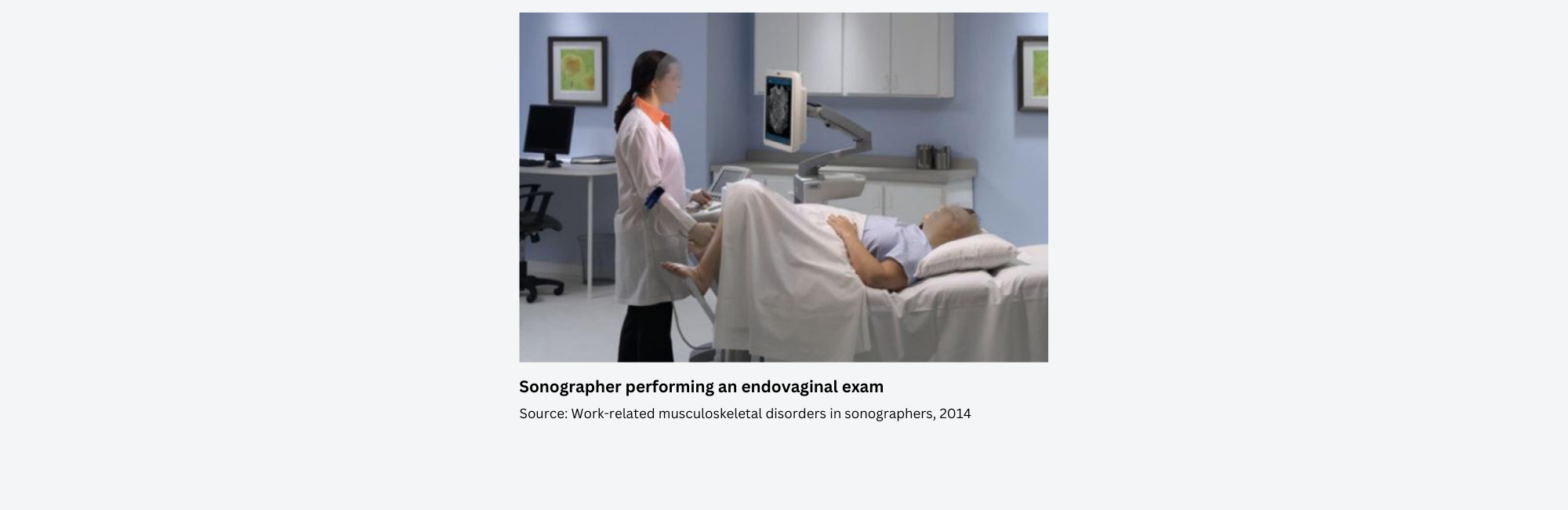
Abdomen & endovaginal scanning
During scannings on the left side of a patient's abdomen, the practitionar must have the patient on her or his side and position to the edge of the exam table toward the sonographer. For endovaginal scans, the sonographer should perfom the screening from the end of the table (Coffin 20).
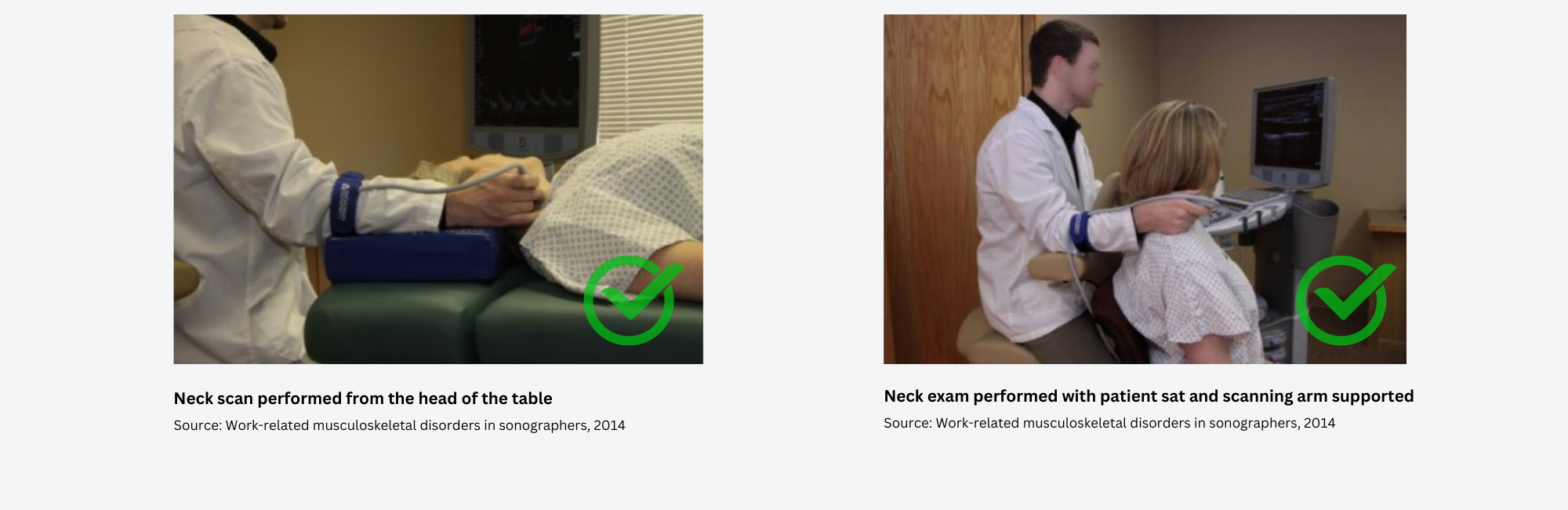
Neck scanning
The recommended position for neck scannings is with the sonographer performing the exam from the head of the table, facing the feet of patient. Another alternatives for these procedures, is with the sonographer sat or standed at the level of the patient's shoulder or having the patient sat in front the sonographer and scan behind him or her (Coffin 20).
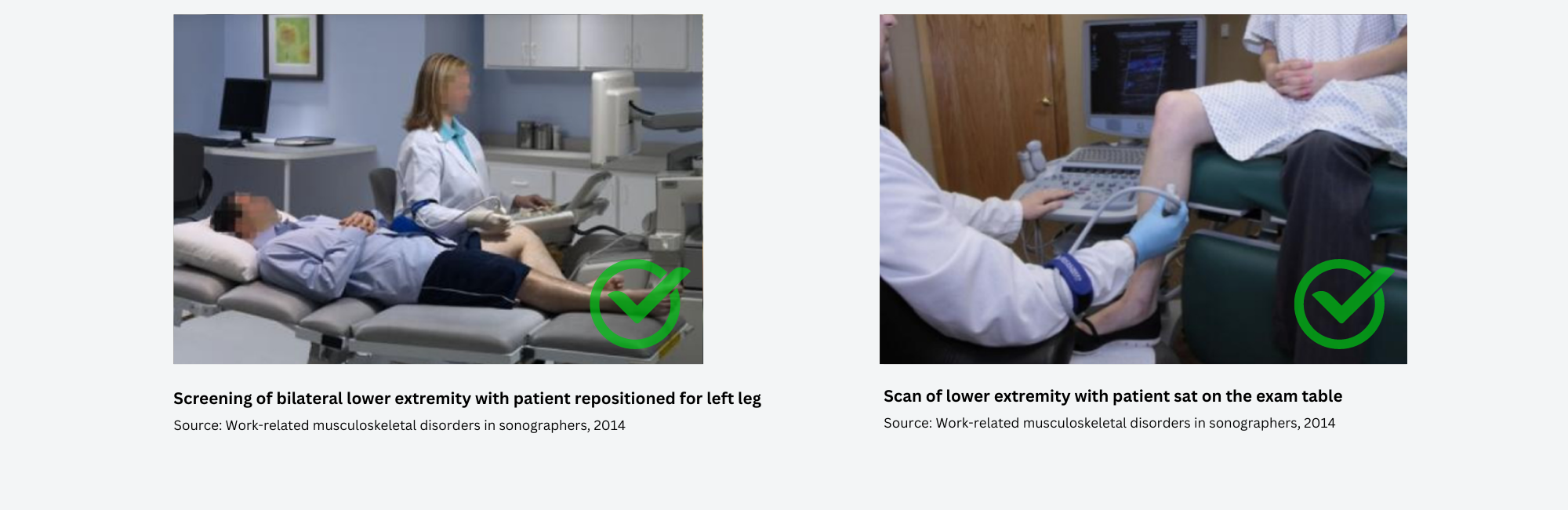
Bilateral/left lower extremity venous exams
For bilateral or left lower extremity venous exams, the patient should turn around on the exam table in a position where their left leg is closest to the sonographer. Other alternative for this type of exam, is with the patient sat with their legs hanging at the edge of the exam table (Coffin 21).
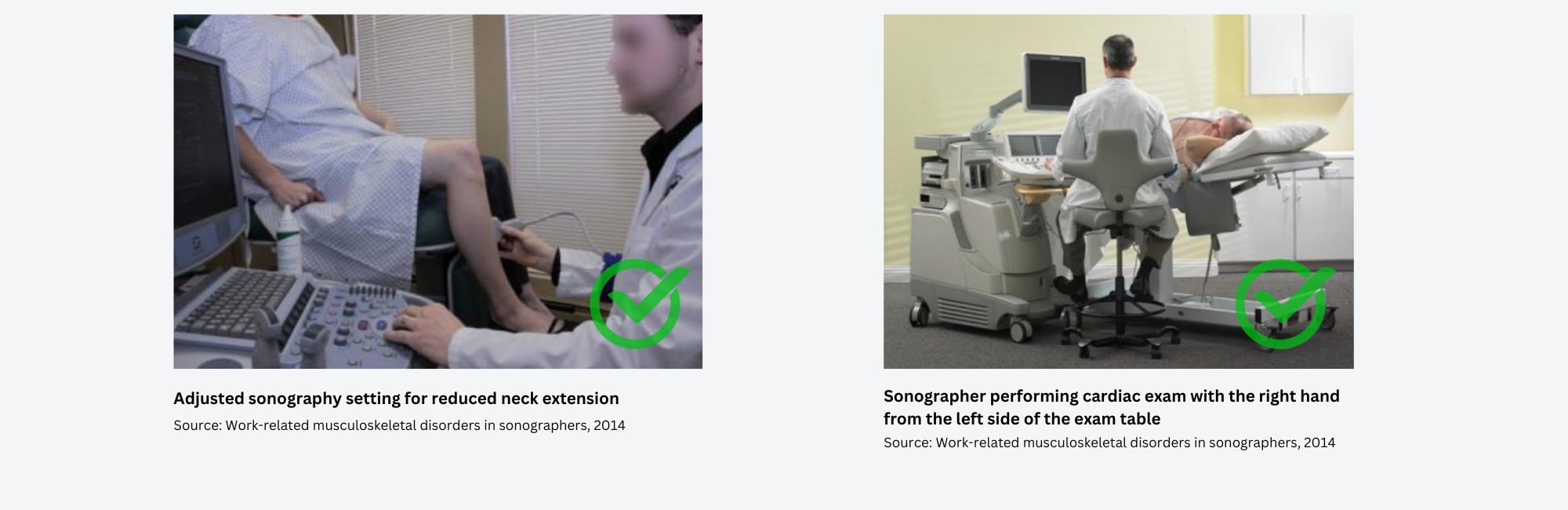
Control panel & monitor
Besides the above, it is important that the ultrasound system's control panel has a wide height range of at least 24 inches, and that is adjustable enough to prevent the sonographer to reach up for the controls, reducing neck extension when viewing the monitor (Coffin 21).
Cardiac scans
For cardiac scans, it is recommended to scan left-handed on the left side of the patient, and for those who prefer to scan with the right hand, the exam should be performed from the left side of the patient but facing the end of the exam table (Coffin 22)
Start Your Day With This WRMSDs Prevention Checklist
- Is the patient close enough to me? Is my arm and elbow tucked in closely to my body in a comfortable position?
- Did I adjust my chair or examination bed according to the body habitus of my patient in relationship to my height?
- Is my posture a comfortable and correct one so as not to cause undue stress on my body?
- Am I working with my wrist and neck in a straight and supported position?
- Is the monitor and keyboard positioned so that I can easily see and reach them?
- Am I supporting my limbs properly throughout the entire examination?
- When I stand, am I carrying my body weight equally on both feet?
- Did I take a micro break? I.e. consciously releasing tension on the scanning hand for a few seconds?
- Did I take a mini-break? I.e. removing the probe from the scanning hand, stretching the hand, arm and shoulders and glancing periodically away from the monitor to release eye tension?
- Am I aware of any unusual symptoms, such as numbness, swelling or pain?
References:
Burnetta, David R. and Campbell-Kyureghyan, Naira H. "Quantification of scan-specific ergonomic risk-factors in medical sonography" International Journal of Industrial Ergonomics Vol. 40, Iss. 3, 306-314 May 2010
https://www.sciencedirect.com/science/article/abs/pii/S0169814109001401
Coffin, Carolyn T. "Work-related musculoskeletal disorders in sonographers: a review of causes and types of injury and best practices for reducing injury risk" Reports in Medical Imaging 15-26 15 Feb 2014
https://pdfs.semanticscholar.org/16c0/b905557242e6eeb9ab51f94b2630003f7937.pdf
Fisher, Thomas F. "Radiologic and Sonography Professionals’ Ergonomics: An Occupational Therapy Intervention for Preventing Work Injuries" Journal of Diagnostic Medical Sonography Vol. 31, Iss. 3 137-147 May/Jun 2015
https://journals.sagepub.com/doi/full/10.1177/8756479315580020
Murphey, Susan "Work Related Musculoskeletal Disorders in Sonography" Journal of Diagnostic Medical Sonography Vol. 33, Iss. 5 354-369 Sep/Oct 2017
https://journals.sagepub.com/doi/full/10.1177/8756479317726767
Murphy, Carmel and Russo, Andre "An Update on Ergonomic Issues in Sonography" Healthcare Benefit Trust Report Jul 2000
https://soundergonomics.com/wp-content/uploads/2020/10/Update_on_Ergo_Issues.pdf